➦ Introduction
What are the four steps of rheumatoid arthritis (RA)? Not only patients but also guardians and anyone else who wants to learn more about this crippling condition need to understand it.
Rheumatoid arthritis (RA) can be mild, moderate, or severe, with symptoms that differ from person to person.
There is no set timetable for how long RA will last. If you don't get good care, the condition will probably get worse over time, going through different stages.
➦ What is Rheumatoid Arthritis?
RA, or rheumatoid arthritis, is an autoimmune and inflammatory disease. This means that your immune system attacks healthy cells in your body by accident, making the affected areas of your body swell and hurt.
The joints are mostly affected by rheumatoid arthritis, which is an autoimmune disease. It's marked by long-lasting swelling and pain in the lining of the joints, which can finally damage the joints.
Lean More About: What Is The Rheumatoid Arthritis
➦ These are the four stages of RA:
Stage 1: Early RA
Stage 2: Mild RA
Stage 3: Severe RA
Stage 4: End Stage RA
rheumatoid arthritis stages, RA symptoms are different and affect both sides of the body equally. Symptoms are usually worst when a person first gets up or after being still for a long time.
In the end, RA symptoms are caused by inflammation in the joints, which affects the synovial tissues that line the joints.
Additionally, as RA gets worse and symptoms get worse, this ongoing inflammation damages more joints, leading to more problems like joints not working properly and limited movement.
People with all stages of RA can take a mix of prescription drugs, over-the-counter (OTC) drugs, and home remedies to control their condition.
➦ Rheumatoid Arthritis Treatment Focuses
- getting rid of pain
- Keeping joints from getting hurt, losing their range of motion, or becoming deformed
- being less likely to lose function
- Keeping up a good standard of living
Prosoma 500mg is great because it can help with pain in many ways. Sleep troubles aren't separate problems; they're often linked to other things going on in the patient's life. People who have trouble sleeping can get a full answer from Prosoma, which looks at physical, social, and environmental factors.
➦ Stages of Rheumatoid Arthritis
The body changes as RA gets worse. There are changes you can see and feel and changes you can't. Different treatment goals are needed for each stage of RA.
➦ Stage 1: Early RA
People with stage 1 RA, also called early RA, often have swelling in their joints, which leads to: joint pain
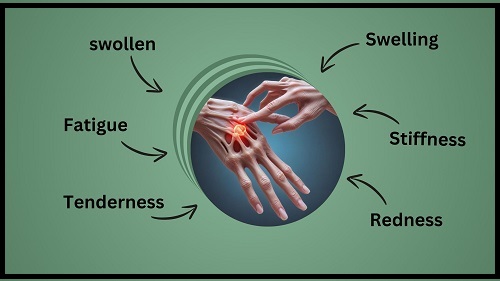
- swelling
- stiffness
- redness
- tenderness
- Fatigue
- swollen
In the early stages of RA, joint damage usually doesn't happen. The best thing that can happen is that a doctor should find and treat early signs of RA within 12 weeks.
Methotrexate is a cancer drug that changes how the immune system responds. It is often one of the first drugs used to treat people with RA. Methotrexate can be taken as a pill or put into a vein.
Disease-modifying antirheumatic drugs (DMARDs) are drugs like methotrexate that change the way the body's immune system works over time.
Most people with RA need more treatments to fully control their symptoms and slow the disease's growth. Some other medical treatments that can help treat and handle stage 1 RA are:
- Nonsteoidal anti-inflammatory drugs (NSAIDs) can be bought over-the-counter or with a prescription. They come in pill, patch, or cream form.
- Medications like methylprednisolone, prednisolone, and prednisone are called corticosteroids.
- the use of physical and occupational therapy.
➦ Stage 2: Mild RA
People with stage 2 RA, also called moderate RA, often have stage 1 symptoms that are worse or last longer, and they also have less mobility or range of motion more often or for longer amounts of time.
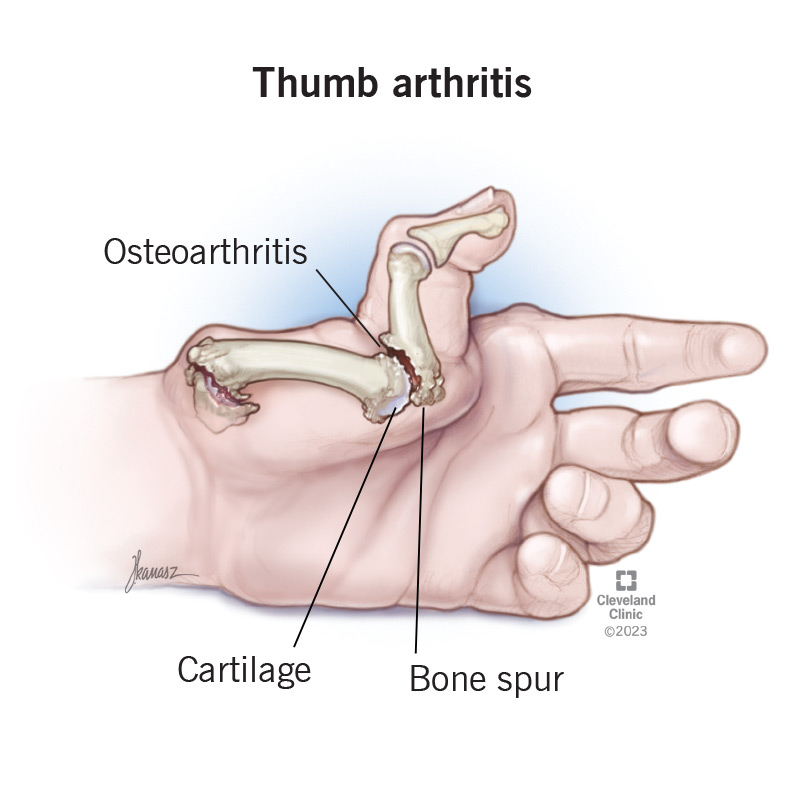
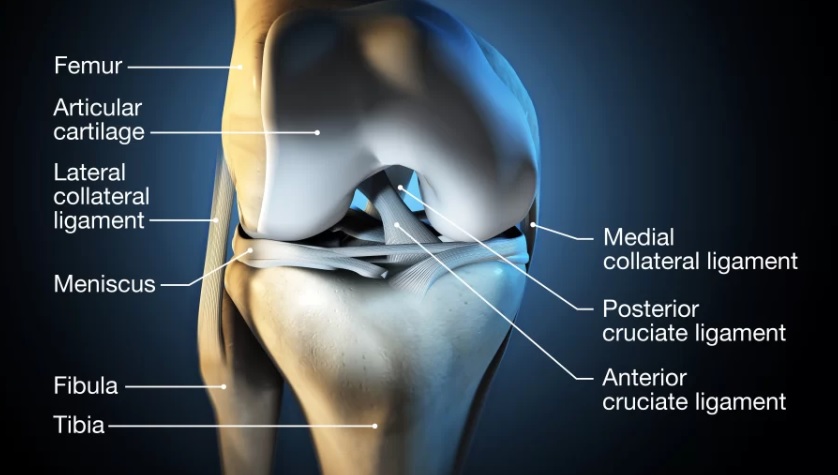
In stage 2 RA, stiffness and swelling in the joints can start to harm the cartilage in the joints.
Once doctors know which joints are most likely to break, they will continue care with other prescription or over-the-counter drugs. Doctors may add another group of drugs called biologic response enhancers to a patient's treatment plan based on how they respond.
➦ Stage 3: Severe RA
When RA gets to stage 3, doctors say it is very bad. Now, the damage has spread to the cartilage, and the bone loss is getting worse. The bones rub against each other because the covering between them wears away.
There could be more pain and swelling. Some people may feel their muscles getting weaker and lose more of their movement.
Damage to the bones can happen (erosion), and the way they are formed may change. Fingers that are twisted and hands that are thickened are examples of damage that may not go away. Other signs may include tendons that are squished at the wrist, which can be a sign of carpal tunnel syndrome or a ruptured tendon.
There is a big chance that the extensor tendons on the fingers will tear because of synovitis at the wrist, but doctors can stop this from happening if they find it early.
➦ Stage 4: End Stage RA

In the fourth stage, there is no longer any swelling in the joint. In this stage of RA, the joints don't work right anymore.
People with end-stage RA may still feel pain, swelling, stiffness, and loss of movement. There might be less muscle power. The joints could get damaged, and the bones could bond together (ankylosis).
People with end-stage RA may lose the use of their hands or have trouble bending their knees or moving their hips, depending on how far along the disease is and where it is located.
It can take years to move through all four steps, and some people don't make it all the way through. Fewer than 0.8 percent of people with RA have fused bones, also known as ankylosis.
Some people with RA don't have any symptoms for a while. This could sometimes mean that the RA is under control.
➦ Signs RA is progressing
For most people with RA, their symptoms get worse over time. RA may get better at times, making it easier to handle. rheumatoid arthritis symptoms may get worse and show up more often at other times.
Your situation will get worse or better depending on many things, such as:
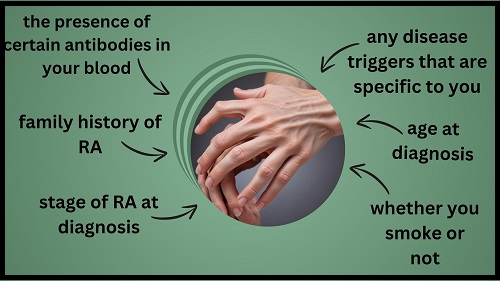
- family history of RA
- age at diagnosis
- stage of RA at diagnosis
- any disease triggers that are specific to you
- the presence of certain antibodies in your blood
- whether you smoke or not
Your doctor can help you better understand how your situation is getting worse by taking these things into account.
Keep in mind, though, that no one can say for sure how RA will grow over time in them. If someone in your family has RA, your condition may not continue the same way as theirs.
In general, it means that the RA disease is no longer active. It is more likely that someone with RA will go into remission if they don't have the disease markers anti-cyclic citrullinated peptide antibody and rheumatoid factor.
How your treatment changes as RA progresses
When treating RA, your doctor will look at different kinds of medications and come up with a plan for you.
Your treatment plan will depend on
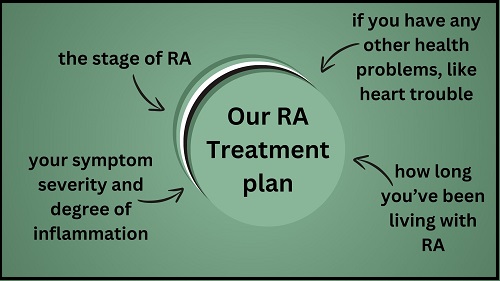
- the stage of RA
- your symptom severity and degree of inflammation
- how long you’ve been living with RA
- if you have any other health problems, like heart trouble
Steroids and nonsteroidal anti-inflammatory drugs can both help lessen inflammation.
Antirheumatic drugs that change the way your body's immune system and inflammatory responses work can help protect joint tissue by slowing the development of RA.
To change the body's inflammatory reaction, biologic drugs work only on the immune system.
When RA gets worse, surgery may be a choice.
The reason for surgery could be to
- improve day-to-day functioning
- reduce pain
- repair damage caused by RA
Surgical objectives could be to
- remove the synovium or nodules
- repair tendons
- fuse joints
- replace a joint entirely
➦ Managing Severe RA
When RA gets really bad, strong drugs like biologic DMARDs can be used to treat it. These work to lower inflammation by going after certain parts of the immune system. Some surgeries, like joint replacement, may also be needed as a last option.
➦ Summary
RA has four different stages, each with a different set of symptoms, limitations in function, and possible complications. Each stage needs to be evaluated in order to find the best treatment and management choices.
10 to 15 percent of people with RA go through recovery. It is important to identify and treat RA early, even though results vary from person to person.
RA may also get better more slowly if you do things like eat well, stop smoking, and hit a healthy weight. People with RA should see a doctor if their joints swell, hurt, or become stiff often or for no reason, or if other symptoms of RA appear.
➦ FAQS
1.How do I know if it’s osteoarthritis or rheumatoid arthritis?
It can be hard to tell the difference between osteoarthritis and rheumatoid arthritis, but it is important to do so in order to get the right treatment. RA is an autoimmune disorder, while osteoarthritis is usually caused by wear and tear on the joints. Imaging and blood tests can help tell the difference between the two types of arthritis.
2.Does osteoarthritis turn into rheumatoid arthritis?
No, osteoarthritis and rheumatoid arthritis are not the same thing. They are two different diseases with different causes. But it is possible for one person to have both types, which can make identification and treatment more difficult.
3.Can an X-ray show the difference between osteoarthritis and rheumatoid arthritis?
Yes, imaging tests like X-rays can help a lot in telling the difference between osteoarthritis and rheumatoid arthritis. For example, people with osteoarthritis may have bone spurs and a shortening of the joint space, while people with rheumatoid arthritis may have joint erosion.